Coronary Procedures
Coronary Angiogram
A coronary angiogram is a procedure performed by a trained cardiologist.
The coronary arteries are small muscular tubes that surround the heart and provide blood flow to it. The heart is a very active organ and requires almost continuous blood flow. A coronary angiogram is designed to check these heart arteries and make sure they are free of blockages.
The procedure is usually performed through a small artery in the wrist but can be performed from the artery in the groin in certain situations. An iodine based dye is used.
Why is a coronary angiogram performed?
- If you have chest pain that the cardiologist feels might be due to a blockage in the coronary artery.
- If you have shortness of breath that the cardiologist feels might be due to a coronary blockage
- Following a positive stress test with or without symptoms
- Prior to heart valve surgery.
- If you have an abnormal heart rhythm
- If you have very high cardiac risk, require a large operation for another reason and are unable or unsuitable for a stress test
Approximately 90% of my coronary angiograms are performed through the wrist. 10% are performed via the artery in the groin. I will explain which is suitable for you and why.
There is very little pain associated with an angiogram. Hence they are performed with local anesthetic and only light sedation. A General anesthetic is only rarely needed.
I require some patients to fast prior to their angiogram. A light breakfast and usual medications are fine.
What are the Risks?
- Bleeding and bruising (more common in procedures from the groin)
- Stroke ( 1 in 1000 to 1 in 2000 patients)
- Heart attack (very rare)
- Cardiac arrest (very rare and almost always reversible)
- Kidney impairment – usually only if the kidney function is not normal prior to the procedure.
What is my Preparation?
- Have a Light breakfast. Fasting isn’t required unless I advise specifically. If unsure ask.
- Kidney function and blood count check via blood tests in the month prior to the procedure
- If you take Warfarin, Eliquis, Pradaxa or Xarelto please let me know and I will provide instructions
- Aspirin, Clopidogrel, Effient, Brilinta can continue.
- All heart medications should continue.
- Metformin (Diabex, Diaformin) or combination tablets containing metformin (for diabetes) needs to be stopped two days prior and two days after an angiogram
- If you take an SLGT 2 inhibitor (e.g. Jardiance, Forxiga, Jardiamet, Xigduo) you must stop this medication two days prior to the angiogram.
- Fluids via a drip for 24 hours prior to the procedure in hospital if your kidney function is not normal
What are the possible outcomes of an angiogram?
There are few
- The arteries are normal and medications only.
- There are only minor blockages and medications only required.
- There are blockages of 50 to 70% and additional testing is required at the same time as the angiogram. This is called a pressure test or FFR
- A blockage or blockages of more than 70% and a stent or stents are required.
- There are numerous diffuse blockages that are best treated with open heart bypass surgery
I will usually follow on by implanting a stent immediately if I feel an equivalent or better result is obtainable with stents over bypass surgery. If it is a borderline case or surgery is clearly better, I tend to stop so that we can discuss the best strategy moving forward. I always like patients to be in control of decisions relating to their health care.
Please find our patient consent form required to be completed by all patients prior to their procedure. Click here to download.
This must be agreed to and completed prior.
Coronary Stenting
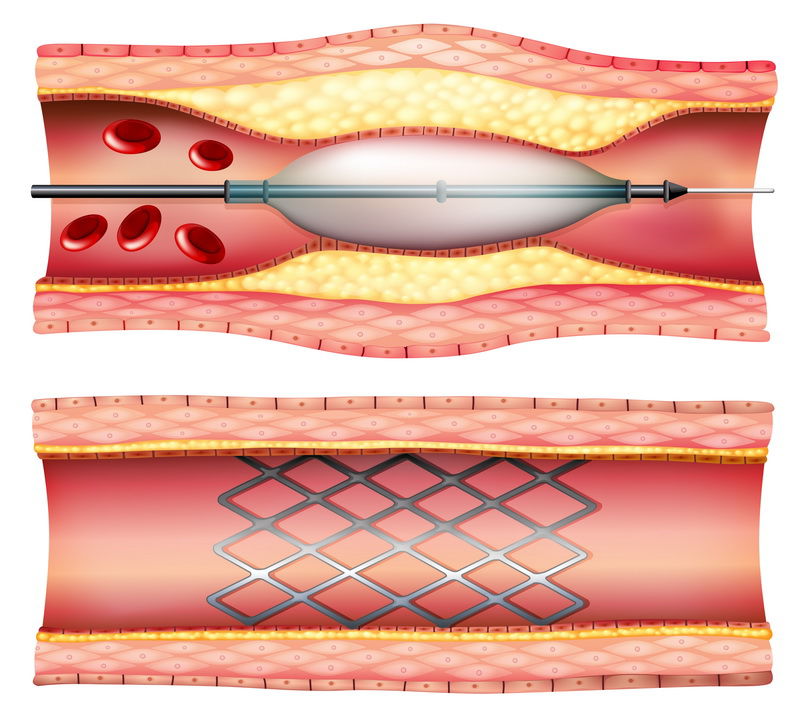
A coronary stent is a metal scaffold that is deployed within a coronary blockage to open the artery and restore normal blood flow. The usual procedure is as follows:
1. The artery is wired with a special coronary guide wire
2. The blockage is usually prepared prior to stenting with a gentle balloon inflation
3. The stent is deployed within the blockage
4. A final balloon within the stent to ensure it is optimally expanded
There are three major types of stents
1. Bare metal stents
2. Drug eluting metal stents
3. Dissolvable scaffolds
Each stent has advantages and disadvantages. One stent may be excellent in one clinical situation but a disaster in another. Drug eluting stents have a lower rate of re-narrowing overtime compared to bare metal stents especially in patients with diabetes or narrow calibre coronary arteries (less than 2.75 mm in diameter). However, drug eluting stents require a minimum of 12 months of blood thinners. Bare metal stents require only 4 weeks. Dissolvable scaffolds are an evolving technology.
This means most surgical procedures will need to be delayed for at least 3 months. If delaying surgery is not an option, a bare metal stent or (drug eluting balloon) may be the best option for you.
Fractional Flow Reserve or FFR
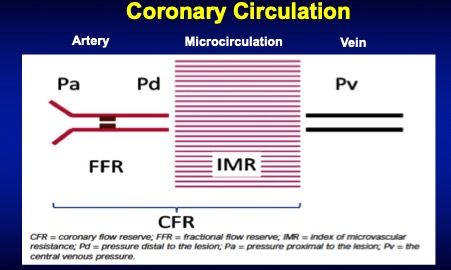
What is it?
A pressure assessment of a coronary narrowing that gives much more information than a % narrowing
Why is it so useful?
Determines who will benefit from a stent and who will not.
Who should have this performed?
Any person with a 50-70% coronary narrowing, to determine if a stent is indicated
Who shouldn't have this performed?
Suitable for almost all patients. AVOID CAFFEINE 24 HOURS PRIOR
Why would I have a narrowed coronary artery and a normal FFR?
The percentage narrowing is an visual estimation of the coronary blockage. It doesn't give any information about whether blood flow is actually reduced to the heart muscle. Very small arteries may have a very significant narrowing e.g. 90% but only a supply a very small part of the heart muscle. These would have a high percentage narrowing and a normal FFR and should not be treated.
What if I have a narrowed coronary artery and the FFR is negative?
These artery should not be stented. The five year risk of heart attack is very low and the risk of stenting outweighs the benefit for most patients.
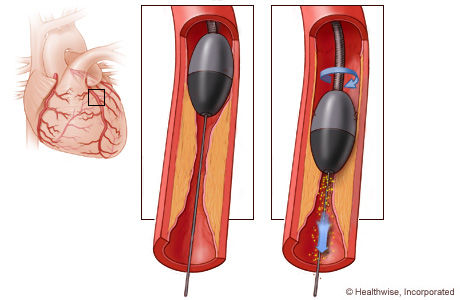
Rotational Atherectomy
What is it?
Rotational atherectomy is a highly specialised catheterization procedure to remove plaque within a blocked or narrowed artery due to a large amount of calcium build up. This is usually performed when balloon angioplasty is not possible or suitable to open up a blocked artery. Rotational atherectomy uses a revolving instrument called a Rotablator to break up calcified plaque clogging a coronary artery in order to restore blood flow to the heart. I offer this service as part of complex coronary intervention to suitable patients.
How it works?
Rotational atherectomy involves navigating a catheter fitted with a Rotablator device (diamond coated burr) through the site of the blockage, where it gently pulverizes the blockage into tiny particles that can pass safely through the bloodstream (particles smaller than red blood cells). Angioplasty and stenting are often performed after rotational atherectomy to improve the results and prevent the artery from re-narrowing.
Why it’s done
As you age your arteries can become clogged from build up of cholesterol plaques and calcium reducing blood flow to heart muscle. This narrowing of the arteries can cause a number of serious heart problems, including:
- Chest pain (angina) or shortness of breath not controlled with medication
- Heart attack
Rotational atherectomy to clear (or debulk) a narrowing artery facilitates balloon angioplasty and stent placement. The procedure can also be used to treat narrowing in the arteries that supply your limbs.
Who Should Perform Rotational Atherectomy?
Extensive training is crucial to the safe implementation of rotational atherectomy. Not all cardiologists can or should be performing this procedure. Watching this procedure is NOT the same as doing it with ones own hands. Being trained by some of Australia's most experience interventional cardiologists with rotablator. I have obtained a high level of practical expertise in this technique.
Always check the credentials and competency of any cardiologist performing this highly specialised procedure.
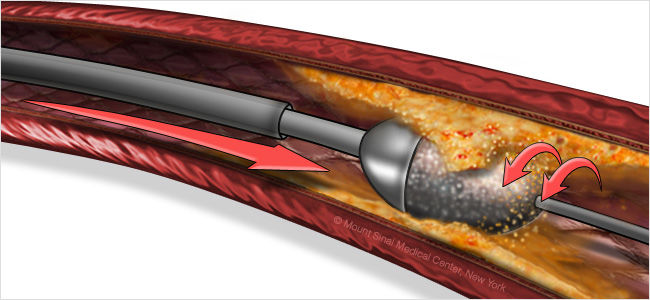
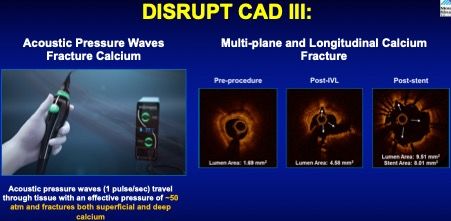
Shockwave Lithotripsy
Shockwave is a novel technique based on an established treatment strategy for renal calculi, in which multiple lithotripsy emitters mounted on a balloon catheter deliver localised pulsatile sonic pressure waves to circumferentially modify vascular calcium altering vessel compliance while maintaining the integrity of the fibro-elastic components of the vessel wall.


Shockwave use in heavily calcified coronary disease (calcium evident either side of coronary lumen on angiography)
- Resistant to balloon inflation (semi-compliant, non-compliant and OPN).
- Greater than 270 degrees of circumferential calcium confirmed on IVUS
- Where sequential rotational atherectomy has failed to adequately modify the calcium to allow stent expansion
- Underexpanded stents implanted in severely calcified lesions
- Where rotational atherectomy is contraindicated
Shockwave use in heavily calcified peripheral artery disease involving iliac, femoral, popliteal, infra-popliteal, mesenteric, celiac or renal arteries
- Resistant to balloon inflation
- Delivery of transfemoral delivery systems e.g. TAVI
Coronary artery IVL balloon catheters are rapid exchange available in 2.5 to 4.0 mm diameters and 12 mm in length and have 2 emitters. Peripheral IVL balloon catheters are over-the-wire balloon ranging from 3.5 to 7.0 mm diameter (0.5-mm increments) and 60 mm in length and have 4 or 5 emitters.
Orbital Atherectomy
Dr Touma is now accredited in orbital atherectomy. This new calcium modification technique offers additional options for patients with heavily calcified coronary artery disease.
As one of the only accredited operators in NSW, you have access to the latest in calcium modification for your coronary disease.
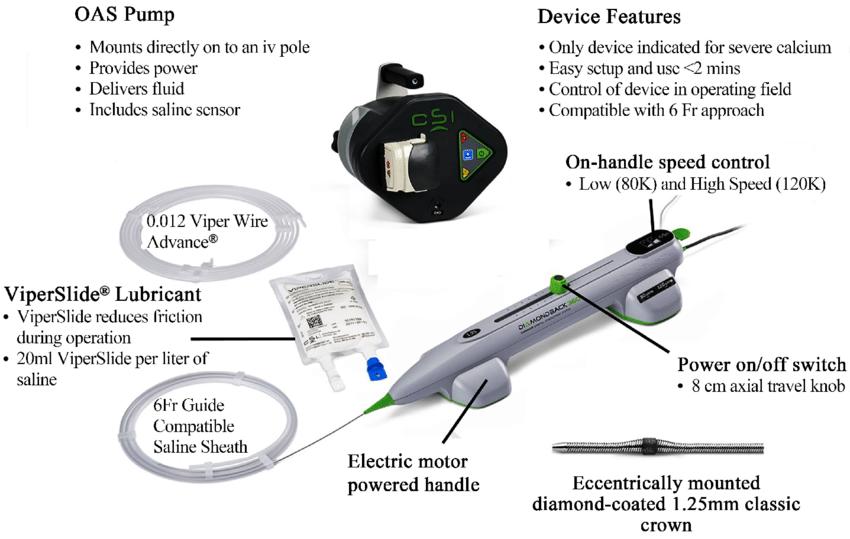
Diamondback 360™ OAS has a Unique Dual Mechanism of Action Design

- The diamond-coated crown sands intimal calcium into particulate with an average size of approximately 2 μm—which is smaller than a capillary vessel.
- With a particulate size of 2 µm and continuous blood flow during orbit, Diamondback 360™ OAS may reduce risk of slow flow and no reflow.
- A single 1.25 mm crown treats vessels 2.5 mm to 4.0 mm through a 6 Fr access.
- The pulsatile impact of the crown against deep plaque can create microfractures that modify deep calcium.
OAS is a First-line Approach for Severe Arterial Calcium
Coronary calcium tends to be underestimated. Calcium considered mild or moderate by angiography may actually be severe if advanced imaging such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT) imaging are used. Moderate to severe arterial calcium is present in 30-40% of patients who undergo a PCI.
Patient Predictors of Arterial Calcification
- Diabetes
- Chronic Kidney Disease
- Advanced Age (>65 y/o)
- Smoker
- Dyslipidemia
- Hypertension
- Prior Coronary Artery Bypass Graft (CABG)
- Known Peripheral Artery Disease (PAD)/Coronary Artery Disease (CAD)
Challenges Associated with Calcium
- Prone to dissection during balloon angioplasty or pre-dilatation
- Difficult to fully dilate the balloon
- May prevent adequate stent expansion and apposition
- May prevent stent delivery
